By: Cat Ebeling, RN, MSN-PHN, co-author of the best-sellers: The Fat Burning Kitchen, The Top 101 Foods that Fight Aging & The Diabetes Fix
Are you at increased risk for bone fractures? The answer is most likely, yes—if you are over the age of 50. You probably have already heard of osteoporosis. This condition bone breakdown at a much higher rate, making your bones more fragile and putting you at a much higher risk of bone fractures.
Osteoporosis can be a silent killer. It’s an often-underdiagnosed condition, discovered when it’s too late to reverse. However, learning to prevent this condition before it develops into full-blown osteoporosis is the key to a longer, healthier life.
Before osteoporosis develops, a bone condition called osteopenia occurs. Osteopenia is a condition of low bone density, meaning the bones are not as strong as they should be. Osteopenia literally means, “poor bones”. Osteopenia often leads to osteoporosis, which is generally very difficult, if not impossible to reverse once your bones get to this point.
Prevention is key.
How Many People Suffer from Osteopenia or Osteoporosis in the United States?
Combined, the estimated number of adults with osteoporosis or osteopenia is 53.6 million, representing approximately 54% of the US adult population ages 50 years or older. A report from the Centers for Disease Control and Prevention also finds that more than four times as many women as men have either osteopenia or osteoporosis. Asian and Caucasian women seem to have the highest tendency towards low bone mass, while African Americans seem to have higher bone density.
The skeleton is made of living, dynamic tissue that requires proper nutrition, exercise, and care that the rest of the body needs for good health. Further, your bones actually play an important role in metabolism, hormone production, blood cell formation, and immune health. Bone health becomes even more critical as we age. Few things in the body are as important to your longevity, mobility, and quality of life–as your bone health.
How Our Bones Grow, Develop and Function
Your skeleton is a living organ that not only provides a protective structure for your soft tissues and organs, but it also serves as the storehouse for essential minerals used by the body.
Bones are continuously in a process of tearing down old bone tissue and growing new bone tissue through a process called remodeling. Bone remodeling involves the removal of older, more brittle, mineralized bone. This older bone is broken down through a process called “resorption” and sent to the kidneys, where it comes out in the urine. New bone matrix is laid down that then becomes hardened and mineralized.
Bone remodeling consists of three phases:
- Resorption, which is when osteoclasts digest old bone and get rid of it.
- Reversal, when mononuclear cells prepare the resorbed surface for osteoblasts, which generate a newly synthesized, bone matrix.
- Formation is the phase when osteoblasts lay down new, stronger, and more resilient bone structure, until the resorbed bone is completely replaced.
This process of bone remodeling adjusts the structure of the bone to meet the changing mechanical needs of the body. In other words, if you are stressing your bones (in a good way) through weight resistance training or running or other weight bearing activities, your body will stimulate new, stronger bone tissue to grow, which helps to strengthen, protect, and repair the existing bone matrix.
Therefore, weight resistance training and other stresses to the bones are the key to prevention of osteoporosis or osteopenia. Bone remodeling goes on all through a person’s life cycle, although peak bone mass usually occurs around of 20-30 years.
Bones also serve as a mineral storehouse which is affected by hormones that respond to changes in blood calcium and phosphorus. When calcium and phosphorus are in short supply in the body, the hormones that regulate these minerals will take them out of the bones to serve more vital functions in other systems of the body. These hormones include parathyroid hormone, calcitriol, growth hormone, cortisol, thyroid hormone, estrogen, progesterone, and testosterone.
When bone loss from excess bone breakdown, combined with low levels of bone rebuilding occur, osteopenia, or ‘thinning’ of the bones occurs, and if this process continues, osteoporosis will be the result. Osteoporosis literally means “porous bones”. This leads to very weak, brittle bones that can easily break with little force. Osteoporosis is officially diagnosed when there is a bone mineral density (BMD) of 2.5 standard deviations below the mean of healthy young individuals.
The scary fact about both osteopenia and osteoporosis is that these bone conditions are usually silent, developing over many years, and going unnoticed, until you experience a bone fracture. With osteoporosis can come major bone breaks, causing problems with healing, mobility, disability, and even life-threatening complications. In the elderly, there is an increased risk of death. About 20 percent of seniors who break a hip are still at high risk of dying within one year.
The most common symptoms of osteoporosis include:
- Fractures, most commonly in the hip, the spine or wrist bones.
- Limited mobility, along with difficulty completing everyday activities.
- Bone pain, which can be both permanent and intense.
- Loss of height or more than one inch.
- Hunched or stooped posture. “Dowager’s hump” which occurs when the vertebrae in the upper back become weaker or develop tiny breaks in the bones.
What Causes Osteopenia and Osteoporosis?
Often, chronic inflammation anywhere in the body can increase the risk of low bone mass. Low bone mass is usually caused by a combination of factors including:
- Being female
- Asian descent or northern European descent; having a small frame or being thin
- Sarcopenia, or low muscle mass
- Celiac disease or non-celiac gluten sensitivity (even undetected gluten sensitivity)
- Chronic inflammation in the body leaching minerals from bones, causing osteoporosis
- Sedentary lifestyle with no stress on the bones
- Diet—High sugar, processed foods, alcohol, soda
- Smoking cigarettes
- Too much calcium in diet or from supplements (higher than 500mg/day) which causes an imbalance in the other important minerals needed for bones
- Decrease in estrogen and progesterone in women (hysterectomy, perimenopause, or menopause), low levels of testosterone in men
- Aging
- High thyroid /hyperthyroid condition
- Nutritional deficiencies in vitamin D, vitamin K2, magnesium, phosphorus, boron, and other trace minerals
- Long term use of certain medications
- High chronic stress levels
- Extreme weight loss, severe dieting, malnutrition, poor protein intake
A variety of other health conditions can also lead to osteoporosis due to the inflammation involved, disease process itself, or medications used. These health conditions include:
- Breast, prostate cancer, or other sex-hormone related cancers
- Diabetes, type 1 or 2
- Hyperparathyroidism
- Cushing’s syndrome
- Inflammatory bowel disease
- Autoimmune diseases including rheumatoid arthritis (RA), lupus, multiple sclerosis, Graves’ disease
- Parkinson’s disease
- Female athlete triad–irregular/absent periods, premature menopause
- AIDS/HIV
- Chronic obstructive pulmonary disease (COPD), including emphysema
- Chronic kidney disease
- Liver disease, including biliary cirrhosis
- Organ transplants
- Spinal cord injuries
In addition, certain medications taken over a long period of time can also decrease bone density. These medications include:
- Corticosteroids
- Thyroid Supplements
- Hormone Blocking Drugs
- Certain Diabetes Medications
- Proton Pump Inhibitors or Antacids
- Mood Stabilizers Containing Lithium
- Some Blood Thinners
- Loop Diuretics
- Some Anticonvulsant Medicines for Epilepsy
- Antiretroviral Therapies
- Tramadol Pain Reliever
Diagnosing Bone Density
Prevention of bone loss is much easier than trying to reverse bone loss—especially when your bones become so thin and brittle that you are diagnosed with osteoporosis. Early diagnosis and monitoring of your bone health is key, especially if you are at risk of any of the above conditions.
Most physicians use a Bone Mineral Density test (BMD) often with a low-energy x-ray called a DEXA scan. Other tests used to help detect bone density include looking at medical history, urine and blood tests and checking inflammation levels in the body.
Conventional Treatment for Osteoporosis
Conventional medical treatment for osteoporosis usually involves prescription medications. There are a wide variety of medications available that act on your bones, your hormones, or other physiological functions. Doctors will also recommend exercise and taking calcium supplements.
Conventional treatment of osteoporosis is usually treated with a class of drugs called Bisphosphonates. These drugs include Fosamax, Boniva, Actonel, Alendronate, Actonel, Atelvia, Reclast, Zometa and more.
Bisphosphonates work by inhibiting the osteoclasts that tear down old bone tissue for resorption. Since osteoporosis is caused by too much bone resorption, bisphosphonates seem to make sense in the treatment of osteoporosis. Bisphosphonates, however, have been noted to have a significant collection of adverse side effects.
Yes, they do help to reduce some vertebral fractures by an average of about 49%. However, vertebral fractures are not the most dangerous type of fractures. Hip and leg fractures are. These kinds of fractures reduce mobility drastically and even with surgery, recovery can be slow, and there is an increased risk of death due to the fracture, the recovery process, and the lack of mobility.
Unfortunately, bisphosphonates are not very good at reducing hip and leg fractures. A review of the published studies with over 27,000 patients, found that taking alendronate (Fosamax) risedronate (Actonel) or etidronate (Didronel) does not reduce hip fracture risk in people who had not previously suffered a hip fracture. And in the cases of Actonel and Didronel, they did not prevent hip, leg, or vertebral fractures.
Other serious adverse effects of bisphosphonates include esophageal bleeding, stomach or esophageal ulcers, death of the jawbone (osteonecrosis) vomiting, bone pain, nausea, and acid reflux.
Bisphosphonates promote bone density by increasing the minerals in the bone. They do not build bones by promoting the connective tissue growth, which is also necessary for healthy bones. Because they inhibit the dynamic bone remodeling and rebuilding stage of bone growth, the bones themselves become hardened—but very brittle—and more prone to breaking.
Consequently, while bisphosphonates seem to help prevent osteoporotic bone fractures in the early years of treatment, beyond 5 years, femur fracture risk increases.
Natural Treatments for Osteopenia and Osteoporosis
The very most important thing you can do for your bone health is prevention. Bone health is critically dependent on getting the proper nutrients in the diet, effective and healthy ‘stress’ on the bones, and supplementing if necessary.
You can prevent bone loss by knowing your bone density, especially early on, so you can catch bone loss and take steps to prevent it. Frequent screening for bone density, every few years past the age of 40, is crucial to catch this bone disease before it gets too far.
It’s also prudent to check inflammation levels since inflammation is one of the leading contributors to bone loss. You can help lower inflammation in the body by avoiding processed foods, omega 6 vegetable oils, sugar, and grains.
Some inflammatory markers to ask your doctor to check include: hs C-Reactive Protein (CRP), erythrocyte sedimentation rate, plasma viscosity, fibrinogen, ferritin, and several other acute phase proteins.
Bones need stress to become stronger and to stay strong. You can place healthy stress on your bones by strengthening your muscles–the muscles pull on the bones, which helps make them stronger. Weight resistance is also an excellent way to stress your bones to add density.
Nutrition and Supplements for Stronger Bones
Calcium–While most conventional doctors will direct you to take in more calcium, calcium is usually not the problem. In fact, people in the United States have one of the highest intakes of calcium, through dairy products and calcium supplements, yet, the US also has one of the highest rates of osteoporosis in the world.
In this study published in the New England Journal of Medicine, Harvard researchers evaluated evidence on dairy consumption and health outcomes, including growth and development, cancer risk, bone health, and body weight.
The conclusion was that high consumption of dairy products does not protect against bone fractures in adults and it may increase the risk for fractures, prostate cancer, and endometrial cancer. Evidence does not support an increase in dairy products for calcium.
Magnesium—In terms of bone health, magnesium is often defined as the forgotten mineral. Magnesium and calcium must exist in the proper balance for bones to absorb these minerals. It is known that a magnesium deficiency will contribute to osteoporosis by acting directly on the bone cells and indirectly by impacting on the secretion and the activity of parathyroid hormone (which governs bone health) and by promoting low grade inflammation.
Evaluating Magnesium/Calcium balance seems to be one of the more important assessments in terms of measuring bone density, but it is often overlooked. Optimizing Mg intake might represent an effective and low-cost preventive measure against osteoporosis in individuals with Mg deficiency (which includes about 80% of the population).
Protein–Protein makes up about half the volume of bone and about one-third of its mass. In healthy bones, the bone matrix is undergoing continuous turnover and remodeling, and an adequate supply of amino acids and minerals are needed to support the formation and maintenance of bone across the life span. Older adults tend to eat less protein than younger people, but because they need to feed not only their muscles–but their bones–older adults should be sure to include plenty of high-quality protein in their diets.
Vitamin K2—Vitamin K2, or menaquinone, is an often-overlooked vitamin which serves a very important role in bone density. While vitamin K1 comes mostly from leafy greens, it is a little more difficult to get vitamin K2 from our diets. Vitamin K2 is found primarily in grass fed dairy, sauerkraut, natto–a Japanese dish made from fermented soybeans, and grass-fed butter, meat, liver, and egg yolks.
Vitamin K2 works with vitamin D to help shuttle calcium in the body out of the blood vessels and into the bones and teeth. Vitamin K2 can lower the risk of cardiovascular damage and improve overall heart health, and bone health. According to this 2015 review article, K2 activates a protein that prevents calcium deposits from forming in the walls of blood vessels. Instead, vitamin K-2 promotes healthy bone mineral density by working with osteocalcin, a protein that binds calcium to bones and teeth.
Vitamin D—Vitamin D is a very important part of bone density. Research shows that inadequate vitamin D intakes can lead to bone demineralization. Low vitamin D levels can lead to decreased calcium absorption and ultimately a release of calcium from the bones to maintain circulating calcium concentrations. Continuous bone turnover and resorption can weaken the structure of the bones and increase the risk of fracture through secondary hyperparathyroidism. This can lead to the development of osteomalacia and osteoporosis.
Omega 3 Fatty Acids– Omega-3 fatty acids found in fish oils have been shown to decrease markers of inflammation and decrease death due to heart disease. Several studies in animals suggest that fish oil (with high levels of EPA and DHA) supplementation inhibits bone break down. Omega 3’s also helps to increase the amount of calcium absorbed from the diet and enhance the calcium placement in the bones.
Anything that causes inflammation will also activate the osteoclasts, the bone cells that break down old and brittle bone material. Once this happens, the osteoblasts are supposed to move in and start rebuilding new bone. However, when inflammation becomes chronic, it causes the bone-breakdown portion of remodeling to go into overtime. Too much osteoclast activity causes more bone thinning.
Your osteoclasts are only supposed to remove old and brittle or damaged bone. A job they do very efficiently. Then, they’re supposed to clear out and let the bone-building osteoblast cells start the more time-consuming job of rebuilding new bone to replace the bone your osteoclasts have removed.
But when inflammation is chronic, bone osteoclasts go into overtime. Since building new bone takes much longer than breaking down old bone, too much osteoclast activity can result in bone thinning (or osteopenia) and, ultimately, in osteoporosis. That’s where the omega 3 fatty acids come in.
Omega 3 fatty acids tune down the inflammatory signaling that causes the accelerated bone breakdown. So, omega 3 fats slow down bone loss and protect the bones.
Collagen—Collagen is a protein found abundantly in the body. It is used to make up the connective tissue, joints, ligaments, and tendons. Collagen is also what provides structure to the skin to help it look younger. Collagen is by far, one of the major substances in the bones.
As we age, collagen production in the body decreases, along with bone mass. Collagen supplements can inhibit the bone breakdown process that can lead to weakened bones and osteoporosis. Collagen also helps the bones retain their resilience and help prevent the brittleness that can occur with bone mass loss.
In this 1-year study, women took a calcium supplement with 5 grams of collagen or the calcium supplement without collagen. At the end of the study, the women taking the collagen had significantly lower blood levels of proteins that promote bone breakdown than those taking only the calcium supplement. One other study found similar results. The women taking the collagen showed an increase of up to 7% in their bone mineral density compared to those not taking collagen.
Hormones—The sex hormones (for men and women) are also extremely important in regulating the growth of the skeleton and maintaining the mass and strength of bone. The female hormones estrogen and progesterone, as well as testosterone, have positive effects on bone health in men and women. These hormones are essential to bone health because they promote the activity of the osteoblasts, the bone building cells. Many women take bioidentical estrogen and progesterone and testosterone to help keep their bones strong. Men often take testosterone to help with bone loss.
What About Calcium?
Your conventional doctor may tell you to take calcium supplements of 1000-1200 mg a day and nothing else. Unfortunately, studies show that calcium supplementation not only throws off the natural balance needed between magnesium and calcium, but it may also collect on the blood vessel walls, the kidneys and other delicate organs.
There may be a link between excessive calcium intake and heart disease. A study published in the British Medical Journal showed calcium supplements associated with an increased risk of myocardial infarction.
A similar controversy surrounds calcium and prostate cancer. Some studies have shown that high calcium intake from dairy products and supplements may increase risk, whereas another more recent study showed no increased risk of prostate cancer associated with total calcium, dietary calcium, or supplemental calcium intakes.
Your best bet is to get calcium from your diet, but you don’t have to load up on dairy foods. In fact, too much dairy can have adverse effects on your health. This well-known study, called Milk and Health, shows the relationship of milk consumption to an increased risk of fracture, obesity, cardiovascular disease, allergies, and various cancers.
Dark leafy greens are one of the best sources of dietary calcium, and they contain a good balancing dose of magnesium, iron, potassium, and manganese. They also provide a good dose of K, C, E and B vitamins. Dark green vegetables also include many powerful phytonutrients including beta-carotene, lutein, and zeaxanthin, which protect our cells from damage and our eyes from age-related problems, among many other effects. Dark green leaves, like kale, and chard even contain small amounts of omega-3 fats. Sardines also provide a good dose of healthy calcium and omega 3 fats as well.
Lifestyle Changes for Your Bones
There are many studies showing how well strength training not only builds muscle but it slows bone loss, and some studies even show resistance training can build bone. This can be a big factor in slowing bone loss, especially for women after menopause.
Any activity that puts stress on the bones can promote bone-building cells to go to work. Stress that comes from the muscles and ligaments tugging and pushing on bones during resistance training will result in stronger, denser bones. Weight bearing exercise like running and walking are also helpful in stressing the bones to become stronger.
Weight training targets the bones of the hips, spine and wrists, sites that often are high risk for fractures. And best of all, weight training increases muscle strength, power, and balance which helps promote mobility, stability and reduces the risk of fractures as well.
Key Points for Better Bone Health
- Bone scans early on (age 30-40) can help to establish a baseline for your bone health. Bone scans should be done regularly starting at age 50 to catch any early signs of bone deterioration—before osteoporosis sets in.
- Don’t smoke cigarettes—they decrease bone mass.
- Avoid eating foods that contain gluten. Gluten can be one of the primary causes of bone loss.
- Eat a healthy diet, including lots of bright colored fresh vegetables, healthy proteins, and healthy fats.
- Avoid processed foods, omega 6 fats, sugar, and grains.
- Go easy on dairy products.
- Work on getting more vitamin K2 in your diet from grass fed butter, cheese, natto, meat and egg yolks.
- Review medications that may speed up bone loss with your physician and avoid taking them for long periods of time.
- Reduce inflammation as much as possible.
- Take additional supplements for bone health.
- Get regular weight bearing or weight resistance exercise. Stress your bones!
Remember preserving your bone health can lead to a longer, healthier life with better mobility!
Speaking about preserving our bone health, ever wonder how our own ancestors fared with their bone health.
While we’re on the topic of your bone density and preventing Osteoporosis, did you know there are 5 common foods that can slowly DISSOLVE your bones?
Yes, they’re really that bad – AVOID these foods if you’re over 60.
==> 5 foods to Avoid for Osteoporosis
 thenutritionwatchdog.com What's in your food? Discover which "healthy" foods are harming your health and which foods protect your body
thenutritionwatchdog.com What's in your food? Discover which "healthy" foods are harming your health and which foods protect your body 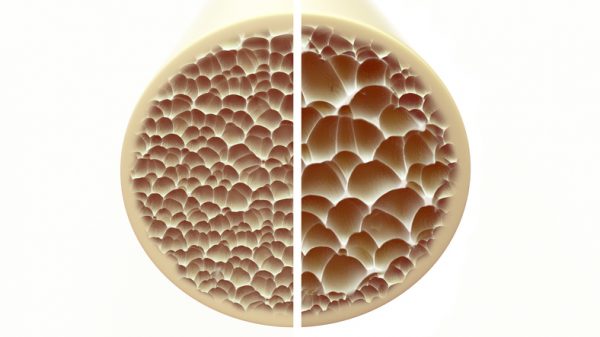

Hi Mike,
What supplements decrease or reverse psoriatic arthritis?
I began taking krill oil about a month ago and I’m seeing improvements.
Do you know whether Back Seed Oil can help?
I also take organic Baobab powder in my smoothie, along with Turmeric, Ashwagandha, raw, organic Cacao, raw organic Beet Root powder, Astragalus, Ginger, Chinese Skullcap, Moringa, Shitake Mushroom, Chaga Mushroom, Matcha, Lion’s Mane Mushroom, and organic Pomegranate juice, and raw goat milk when I have it.
You make me feel so unhealthy. !!!